[1]SUN Yubo,LI Haitao,SHU Zhilin,et al.A quantitative gait assessment method based on lateral gastrocnemius sEMG for neuromodulation of Parkinson’s disease[J].CAAI Transactions on Intelligent Systems,2022,17(1):98-106.[doi:10.11992/tis.202103045]
Copy
A quantitative gait assessment method based on lateral gastrocnemius sEMG for neuromodulation of Parkinson’s disease
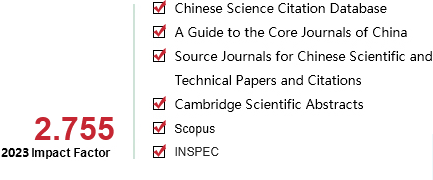
CAAI Transactions on Intelligent Systems[ISSN 1673-4785/CN 23-1538/TP] Volume:
17
Number of periods:
2022 1
Page number:
98-106
Column:
学术论文—智能系统
Public date:
2022-01-05
- Title:
- A quantitative gait assessment method based on lateral gastrocnemius sEMG for neuromodulation of Parkinson’s disease
- Keywords:
- deep brain stimulation; Parkinson’s disease; quantitative assessment; gait variability; sEMG; neural activation; muscle activation; plantar-pressure
- CLC:
- TP249;TP274
- DOI:
- 10.11992/tis.202103045
- Abstract:
- Deep brain stimulation (DBS) is proven to be an effective neuromodulation treatment method for Parkinson’s disease (PD), and there is an urgent need for objective and quantitative assessment during neuromodulation treatment. In this work, a gait assessment method based on lateral gastrocnemius (LG) surface electromyogram (sEMG) signals is designed. The low-frequency trend in sEMG signals is removed by a smooth a priori algorithm, while important information related to PD motion abnormality is retained. The wavelet transform analysis is performed to detect heel strike and recognize gait cycle, and the sEMG data can be accordingly segmented. Then, the variability indices on neural activation and muscle activation are extracted. A gait quantitative assessment system is established, using wireless wearable equipments to synchronously acquire the sEMG and plantar pressure data. Ethical approval is granted and clinical study is conducted on PD patients treated with DBS. The proposed indices have high consistency with the traditional gait cycle time variability index, verifying effectiveness of the proposed method. What’s more, the proposed sEMG variability indices show higher discrimination capability.
- References:
-
[1] LANG A E, LOZANO A M. Parkinson’s disease[J]. The new England journal of medicine, 1998, 339(16): 1130–1143.
[2] JANKOVIC J. PANKOVIC J. Parkinson’s disease: clinical features and diagnosis[J]. Journal of neurology, neurosurgery & psychiatry, 2008, 79(4): 368–376.
[3] SVEINBJORNSDOTTIR S. The clinical symptoms of Parkinson’s disease[J]. Journal of neurochemistry, 2016, 139(S1): 318–324.
[4] 许梦圆, 陈涛, 孟徐, 等. 帕金森病运动症状量化评估的研究进展[J]. 中华神经科杂志, 2020, 53(10): 845–854.XU Mengyuan, CHEN Tao, MENG Xu, et al. Progress on quantitative assessments of motor symptoms for Parkinson′s disease[J]. Chinese journal of neurology, 2020, 53(10): 845–854.
[5] TOLOSA E, WENNING G, POEWE W. The diagnosis of Parkinson’s disease[J]. The lancet neurology, 2006, 5(1): 75–86.
[6] BOUTHOUR W, MéGEVAND P, DONOGHUE J, et al. Biomarkers for closed-loop deep brain stimulation in Parkinson disease and beyond[J]. Nature reviews neurology, 2019, 15(6): 343–352.
[7] LOZANO A M, LIPSMAN N, BERGMAN H, et al. Deep brain stimulation: current challenges and future directions[J]. Nature reviews neurology, 2019, 15(3): 148–160.
[8] 牛朝诗, 熊赤. 脑深部电刺激术治疗运动障碍性疾病现状与展望[J]. 中国现代神经疾病杂志, 2020, 20(12): 1027–1031.NIU Chaoshi, XIONG Chi. The achievement and prospect of deep brain stimulation for the treatment of movement disorders[J]. Chinese journal of contemporary neurology and neurosurgery, 2020, 20(12): 1027–1031.
[9] CHEN Shengdi, GAO Guodong, FENG Tao, et al. Chinese expert consensus on programming deep brain stimulation for patients with Parkinson’s disease[J]. Translational neurodegeneration, 2018, 7(1): 1–8.
[10] KOEGLSPERGER T, PALLEIS C, HELL F, et al. Deep brain stimulation programming for movement disorders: current concepts and evidence-based strategies[J]. Frontiers in neurology, 2019, 10: 410–419.
[11] 李青青, 吴宗耀. 步行中胫前后肌群的表面肌电图[J]. 神经损伤与功能重建, 2007(2): 116–119.LI Qingqing, WU Zongyao. Surface electromyography of the anterior and posterior tibial muscles during walking[J]. Neural injury and functional reconstruction, 2007(02): 116–119.
[12] MIRELMAN A, BONATO P, CAMICIOLI R, et al. Gait impairments in Parkinson’s disease[J]. The lancet neurology, 2019, 18(7): 697–708.
[13] BAILEY C A, CORONA F, MURGIA M, et al. Electromyographical gait characteristics in Parkinson’s disease: effects of combined physical therapy and rhythmic auditory stimulation[J]. Frontiers in neurology, 2018, 9: 211.
[14] KELOTH S M, RADCLIFFE P J, RAGHAV S, et al. Differentiating between Parkinson’s disease patients and controls using variability in muscle activation during walking[C]//2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society . Montreal, Canada, 2020: 3158–3161.
[15] CANTú H A, NANTEL J, MILLáN M, et al. Abnormal muscle activity and variability before, during, and after the occurrence of freezing in Parkinson’s disease[J]. Frontiers in neurology, 2019, 10: 951.
[16] ALDAYIL E, KERR A. Plantarflexor muscle activity during a change in walking speed on a treadmill: comparison between Parkinson’s and unimpaired controls[J]. Physiotherapy, 2021, 113: e96–e97.
[17] BUCHANAN T S, LLOYD D G, MANAL K, et al. Neuromusculoskeletal modeling: estimation of muscle forces and joint moments and movements from measurements of neural command[J]. Journal of applied biomechanics, 2004, 20(4): 367–395.
[18] MOON Y, SUNG J, AN Ruopeng, et al. Gait variability in people with neurological disorders: a systematic review and meta-analysis[J]. Human movement science, 2016, 47: 197–208.
[19] CASAMASSIMA F, FERRARI A, MILOSEVIC B, et al. A wearable system for gait training in subjects with Parkinson’s disease[J]. Sensors, 2014, 14(4): 6229–6246.
[20] HAUSDORFF J M, CUDKOWICZ M E, FIRTION R, et al. Gait variability and basal ganglia disorders: stride-to-stride variations of gait cycle timing in Parkinson’s disease and Huntington’s disease[J]. Movement disorders, 1998, 13(3): 428–437.
[21] 刘姁霖, 王丹, 杨伟伟. 步态训练在帕金森病康复治疗中的研究进展[J]. 中国康复医学杂志, 2019, 34(3): 354–359.LIU Xulin, WANG Dan, YANG Weiwei. Research progress of gait training in the rehabilitation of parkinson’s disease[J]. Chinese journal of rehabilitation medicine, 2019, 34(3): 354–359.
[22] KONRAD P. The ABC of EMG: a practical introduction to kinesiological electromyography[M]. Scottsdale: Noraxon USA. Inc., 2005: 30–35.
[23] RISSANEN S, KANKAANP?? M, TARVAINEN M P, et al. Analysis of surface EMG signal morphology in Parkinson’s disease[J]. Physiological measurement, 2007, 28(12): 1507–1521.
[24] AL OMARI F, HUI Jiang, MEI Congli, et al. Pattern recognition of eight hand motions using feature extraction of forearm EMG signal[J]. Proceedings of the national academy of sciences, India section A: physical sciences, 2014, 84(3): 473–480.
[25] PHINYOMARK A, LIMSAKUL C, PHUKPATTARANONT P. Application of wavelet analysis in EMG feature extraction for pattern classification[J]. Measurement science review, 2011, 11(2): 45–52.
[26] BALASUBRAMANIAN V, ADALARASU K. EMG-based analysis of change in muscle activity during simulated driving[J]. Journal of bodywork and movement therapies, 2007, 11(2): 151–158.
[27] YOCHUM M, BINCZAK S. A wavelet based method for electrical stimulation artifacts removal in electromyogram[J]. Biomedical signal processing and control, 2015, 22: 1–10.
[28] ZHANG Jian, SOANGRA R, E LOCKHART T. A comparison of denoising methods in onset determination in medial gastrocnemius muscle activations during ttance[J]. Sci, 2020, 2(3): 53–66.
- Similar References:
Memo
-
Last Update:
1900-01-01